What is the Disc-FX System?
The Disc-FX® System is an innovative, minimal access spine system designed to efficiently access the damaged disc without injury to surrounding disc anatomy. Disc-FX® permits multiple treatment options compared to other ‘single treatment’ devices in the marketplace. In addition to manual decompression, Disc-FX® can help to clean the disc and seal tears in the annulus.
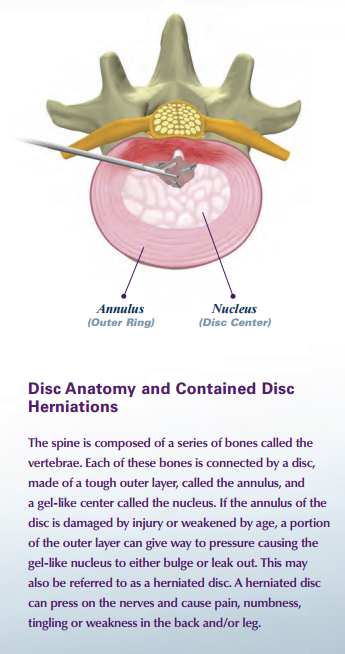
Treating Contained Disc Herniations
In the past, patients with contained disc herniations have been treated with conservative care including rest, medications, injections and/or physical therapy. Unfortunately, this does not always provide relief. In the past, people who did not respond to conservative care were forced to live with the symptoms or consider major spine surgery. If they underwent surgery, it could take weeks or months to recover, causing a major disruption in their daily lives. With Disc-FX®, this is not the case. Disc-FX® provides an option for those people who have failed conservative care, and are not yet ready for major surgery. It is a minimal access procedure performed on an out-patient basis whereby the patient will go home the same day as the procedure with only a small bandage on their back. Following manual removal of the offending herniation, the patented Disc-FX® device is activated to help clean the disc and seal tears in the annulus. As a result, pressure in the disc is reduced, which eases symptoms.
Who is a Candidate for the Procedure?
Patients with symptomatic, contained lumbar disc herniations that have not responded to conservative treatment, may experience relief from the use of Disc-FX®. Typical signs of a contained lumbar disc herniation is lower back pain or pain radiating down the leg accompanied by some lower back pain. Disc-FX® may not be beneficial for advanced degenerative disc disease or spinal fractures. Your doctor will evaluate and determine if you are a candidate for Disc-FX®.
Potential Benefits of the Procedure:
Out-patient procedure • Short procedure time • Local Anesthetic • Minor Skin Incision • Minimal Access Procedure • Multiple Treatment Options • Quick Relief of Symptoms • Can Treat Multiple Disc Levels • Earlier return to normal activities • Preserves all additional surgical options, should they be needed.
Prior to the Procedure
Medical evaluation includes a physical exam. Diagnostic tests such as MRI (magnetic resonance imaging), steroid injection, or discography may be conducted to diagnose and locate the symptomatic disc herniation and determine if the procedure is appropriate
During the Procedure
The Disc-FX® System requires the patient to lie on their stomach throughout the procedure. Minimal anesthesia requirements are typically necessary. A needle is inserted into the skin near the affected disc level, followed by an incision through which a working ‘tube’ is placed. Graspers are used to manually remove and decompress the offending herniation. The patented Trigger-Flex® can then be used to help clean the disc and seal tears in the annulus. At the conclusion of the procedure, the ‘tube’ is removed and a small bandage is applied over the sutures
After the Procedure
Patients are required to remain at the facility after the procedure for observation which is typically one to two hours. Upon release, patients are then informed to rest for one to three days with limited sitting or walking. In most cases, symptoms caused by the disc herniation are gone or diminished within two weeks. A patient may experience some discomfort or bruising where the incision was created. After about one week, patients participate in physical therapy which is important for a full recovery. They are typically allowed to engage in some physical activity and return to work. Your physician will provide a comprehensive recovery schedule
Facet joint disease or deterioration is the most common cause of chronic back pain, and it has been historically difficult to help patients that do not respond to non-surgical treatment without major surgery. Facet joints are paired stabilizing joints located at every level of the spine. They consist of two opposing bony surfaces that are lined by a layer of cartilage.
A capsule surrounding the joint helps to stabilize the spine and contains a lubricating fluid known as synovial fluid. The joints combine with the disc space to create a three-joint complex that prevents excessive spinal motion to protect the spinal cord travelling within the backbone.
TruFUSE® is a new treatment option that is less complex, much less destructive, does not preclude other options and can be used much earlier than major surgery. It is appropriate for many patients who had no other option in the past. TruFUSE® uses two very small, precision tapered dowels that are inserted between facet joints using a special technique to stop them from moving.
Because stopping facet joints from moving stops the entire spinal segment from moving, TruFUSE® is also used as a conservative means to supplement many other procedures when more aggressive fixation is not required.
The TruFUSE® technique minimizes tissue destruction and typically results in minor post-operative pain.
Other treatment methods of facet disease and pain can be used, but many are short-term answers to a long-term problem. Back pain sufferers often initially try clinical solutions such as pain medication, physical therapy, steroid injections, and acupuncture or laser ablation. Traditional fusion, with a deep incision, is often completed by placing pedicle screws into the vertebrae and connecting them with metal rods, resulting in a major surgery and loss of time from work.
The entire procedure, when not used to supplement other, more invasive surgeries, is performed through two small incisions. Muscle tissue is progressively spread apart to reach the facet joints, where a tunnel is created in between the joint and a dowel is inserted. One benefit of the tunnel is that the nerve leading to the joint is removed in that section, which is why most patients find their original pain completely gone immediately after the procedure.
TruFUSE® has been used to treat thousands of patients who had no other option than to continue to suffer safely and effectively. A retrospective study of TruFUSE® outcomes from six different doctors showed that 80 of 81 patients had good to excellent results from the procedure.